Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
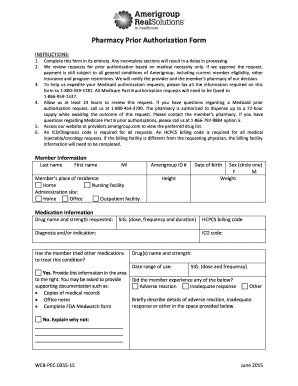
What is the purpose of regence prior authorization form?
The purpose of a Regence prior authorization form is to ensure that a patient receives medically necessary services that are covered under their health plan. The form helps health plans make sure that the service being requested is covered, medically necessary, and that the provider is appropriately licensed and qualified. It also helps to ensure that the services are cost effective and that the patient has met any cost sharing requirements.
When is the deadline to file regence prior authorization form in 2023?
The specific deadline for filing a Regence prior authorization form in 2023 will depend on your plan and provider. You should contact your plan and provider to get specific information about the deadline.
What is regence prior authorization form?
Regence prior authorization form is a document used by health insurance companies, such as Regence BlueCross BlueShield, to determine whether a particular medical treatment, medication, or procedure is covered under a customer's insurance plan. Prior authorization is usually required for costly or non-standard treatment options to ensure they meet the insurance company's coverage criteria. The form is typically filled out by a healthcare provider or pharmacy and submitted to the insurance company for approval before the planned treatment can take place.
Who is required to file regence prior authorization form?
Regence prior authorization forms are typically required to be filed by healthcare providers or medical facilities. This form is used to request approval for specific medical treatments, procedures, medications, or services, ensuring that they are medically necessary and eligible for coverage under Regence insurance plans. It is the responsibility of the healthcare provider or facility to initiate the prior authorization process by submitting the required form.
How to fill out regence prior authorization form?
To fill out a Regence prior authorization form, follow these steps:
1. Obtain the most recent version of the prior authorization form. You can typically find this form on the Regence website or request it from their customer service.
2. Read the instructions carefully. Make sure you understand the purpose of the form and the information required.
3. Provide the general information about the patient, including their name, date of birth, gender, and contact information. Make sure the information is accurate and up-to-date.
4. Fill out the healthcare provider information section, which includes the name, address, phone number, and National Provider Identifier (NPI) of the prescribing healthcare professional.
5. Fill in the details of the requested medication or treatment. Include the drug name, dosage, frequency, and duration of the treatment. If applicable, you may also need to provide the reason for the request and any relevant clinical information or medical history.
6. Attach any supporting documents that may be required, such as medical records, lab reports, or clinical notes. These documents can help justify the request and provide additional context.
7. If necessary, indicate any alternative treatments that have been tried or considered prior to this specific request. This information can help insurers assess the medical necessity of the treatment.
8. Provide the member's insurance information, such as their policy or group number, and any additional information necessary to process the prior authorization request.
9. Review the completed form for accuracy and to ensure all required fields are filled correctly. Any missing or incomplete information may cause delays in the approval process.
10. Submit the completed form to the appropriate entity. This may involve emailing or faxing the form to the specified contact, or following the specific submission instructions provided on the form.
Remember to keep a copy of the completed form for your records. If needed, contact Regence customer service or the prescribing healthcare professional for any further guidance or assistance with the prior authorization process.
What information must be reported on regence prior authorization form?
The specific information that must be reported on a Regence prior authorization form may vary, but generally, the following information is commonly required:
1. Patient information: This typically includes the patient's name, date of birth, contact information, and insurance ID number.
2. Prescriber information: This includes the name, contact information, and credentials of the healthcare provider prescribing the medication or treatment.
3. Medication or treatment details: The specific drug or treatment being requested, including the dosage, strength, frequency, and duration.
4. Diagnosis and medical necessity: The medical condition or diagnosis for which the medication or treatment is being requested, along with any supporting documentation or medical records that justify the medical necessity.
5. Failed therapy or alternative treatments: Any previous or alternative therapies that the patient has tried and failed, including the reasons why they were not effective or caused adverse effects.
6. Supporting documentation: Any relevant medical records, test results, lab reports, imaging studies, or other supporting documentation that provides additional information about the patient's condition and treatment history.
7. Time-sensitive nature: If the prior authorization request is time-sensitive due to the patient's health condition or urgent need, this should be clearly indicated on the form.
8. Signature and date: The prescribing healthcare provider's signature and date, certifying the accuracy and completeness of the information provided.
It's important to note that the exact requirements may differ depending on the specific Regence insurance plan and the type of medication or treatment being requested. It is recommended to refer to the specific prior authorization form provided by Regence or contact them directly for the most accurate and up-to-date information.
How can I manage my regence prior authorization form pdf directly from Gmail?
You can use pdfFiller’s add-on for Gmail in order to modify, fill out, and eSign your regence medication prior authorization form pdf along with other documents right in your inbox. Find pdfFiller for Gmail in Google Workspace Marketplace. Use time you spend on handling your documents and eSignatures for more important things.
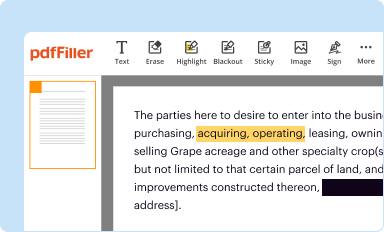
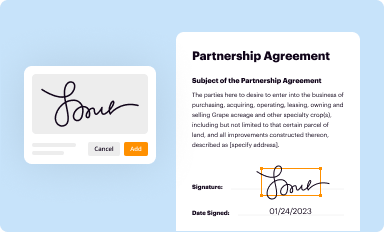
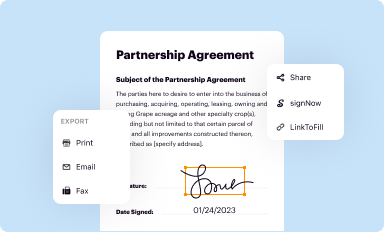
How do I execute regence prior authorization form online?
pdfFiller makes it easy to finish and sign regence blue shield washington prior authorization form online. It lets you make changes to original PDF content, highlight, black out, erase, and write text anywhere on a page, legally eSign your form, and more, all from one place. Create a free account and use the web to keep track of professional documents.
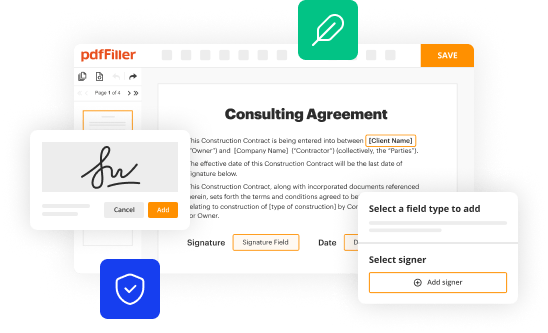
How can I edit regence blue cross blue shield prior authorization form on a smartphone?
You can easily do so with pdfFiller's apps for iOS and Android devices, which can be found at the Apple Store and the Google Play Store, respectively. You can use them to fill out PDFs. We have a website where you can get the app, but you can also get it there. When you install the app, log in, and start editing regence medication prior authorization form, you can start right away.